Life and Dollars: A Health Care Insider’s Account of how Prior Authorization Really Works
By: Wendell Potter (Substack)
February 7, 2023
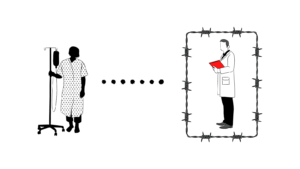
Prior authorization started out as a means by the “payers” of health care goods and services to provide patients the assurance that what their doctors order is medically necessary and appropriate. A strong argument could be made that there is a legitimate role for prior authorization in some circumstances, but big insurers not only have used it to avoid paying for necessary care, but they–and a cottage industry of consultants representing health care providers–have also figured out how to profit from the process. As a consequence, an enormous amount of the money we spend on health care is all too often being used against us, endangering our lives. Below, an executive who ran a prior auth shop pulls the curtains back to explain how it really works. To help the writer avoid potential legal and career problems, we have agreed to publish the piece anonymously.
Journalist Libby Watson assisted with the production of this piece.
Requiring patients to get prior authorization from an insurance company for medical procedures and drugs was supposed to lower medical costs. The theory was that it would prevent doctors from charging for unnecessary care.
The process frustrates patients and burdens health-care providers. And, the numbers show, it doesn’t really work.
I worked at one of the largest prior-authorization companies, running a team that supported the non-clinical side of our business.
It may surprise people to know that many of the biggest health-insurance companies outsource their prior authorization programs. In fact, it would probably shock most people to understand just how much middle management exists between their doctor’s decisions and their ability to receive care. The commercial health insurance industry is overrun with opportunistic companies who profit off our complicated health care system, adding costs that lead to higher premiums and cost of care.
Prior authorization is meant to ensure that a procedure is clinically appropriate, or medically necessary, to cut down on what’s called ‘overutilization’ in the industry. It’s well-established that doctors feel prior authorization puts a huge burden on them, leading to delays in care and adverse health outcomes.
READ FULL ARTICLE HERE
