Why Doctors and Pharmacists Are in Revolt
By Noam Scheiber
December 3, 2023
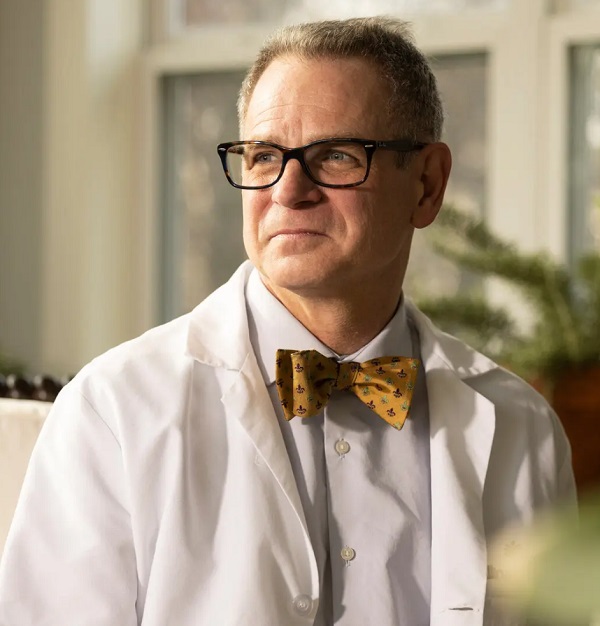 Dr. John Wust does not come off as a labor agitator. A longtime obstetrician-gynecologist from Louisiana with a penchant for bow ties, Dr. Wust spent the first 15 years of his career as a partner in a small business — that is, running his own practice with colleagues.
Dr. John Wust does not come off as a labor agitator. A longtime obstetrician-gynecologist from Louisiana with a penchant for bow ties, Dr. Wust spent the first 15 years of his career as a partner in a small business — that is, running his own practice with colleagues.
Long after he took a position at Allina Health, a large nonprofit health care system based in Minnesota, in 2009, he did not see himself as the kind of employee who might benefit from collective bargaining.
But that changed in the months leading up to March, when his group of more than 100 doctors at an Allina hospital near Minneapolis voted to unionize. Dr. Wust, who has spoken with colleagues about the potential benefits of a union, said doctors were at a loss on how to ease their unsustainable workload because they had less input at the hospital than ever before.
“The way the system is going, I didn’t see any other solution legally available to us,” Dr. Wust said.
At the time he and his colleagues voted to unionize, they were one of the largest groups of private-sector doctors ever to do so. But by October, that distinction went to a group that included about 400 primary-care physicians employed in clinics that are also owned by Allina. The union that represents them, the Doctors Council of the Service Employees International Union, says doctors from dozens of facilities around the country have inquired about organizing over the past few years.
And doctors are not the only health professionals who are unionizing or protesting in greater numbers. Health care workers, many of them nurses, held eight major work stoppages last year — the most in a decade — and are on pace to match or exceed that number this year. This fall, dozens of nonunion pharmacists at CVS and Walgreens stores called in sick or walked off the job to protest understaffing, many for a full day or more.
The reasons for the recent labor actions appear straightforward. Doctors, nurses and pharmacists said they were being asked to do more as staffing dwindles, leading to exhaustion and anxiety about putting patients at risk. Many said that they were stretched to the limit after the pandemic began, and that their work demands never fully subsided.
[READ FULL ARTICLE HERE]
