How PBMs Took Over the Prescription Drug Chain — And Left Patients and Pharmacists Paying the Price
By Luke Sullivan
Apr 02, 2025
 Americans spent a record $464 billion last year on prescription drugs, according to recent numbers from the Centers for Medicare & Medicaid Services.
Americans spent a record $464 billion last year on prescription drugs, according to recent numbers from the Centers for Medicare & Medicaid Services.
Five years ago that number was $335 billion and a decade ago $298 billion. The dramatic increase is not matched by the number of prescriptions filled by pharmacists during that same span.
The average prescription in 2014 was $69. In 2019 it was $76. In 2024 it was $95. This increase has drawn the ire of Congress, which is calling for reforms. Specifically, officials want to rein in the powers of pharmacy benefit managers (PBMs) and how they set prescription drug prices.
“What PBMs are doing to our health care system is criminal,” said Rep. Buddy Carter (R-Georgia), who was also once a pharmacist.
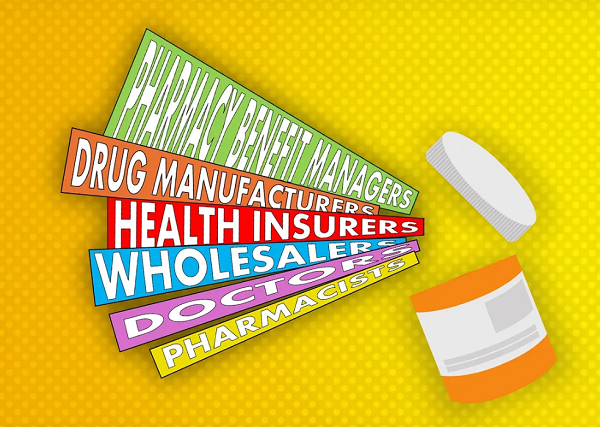
PBMs are middlemen in the drug supply chain. They are a department within every major health insurer in the United States and profit off nearly every prescription filled. Those on prescription drugs – which is two-thirds of all U.S. adults – don’t ever see or likely talk to their PBM. But since the early 2000s these middlemen have had a crucial role in the price of drugs with little oversight.
A big reason why is the cloaked and complicated medical jargon the industry uses to describe the drug supply chain. Many Americans have their health insurance chosen by their employer. It is up to the employer to decide which plan is best. That decision by CEOs is often dictated by price breaks and incentives offered by health insurers.
So at what point do PBMs become part of the drug supply chain?
(Hint: Doesn’t take too long.)
Drug manufacturers help create, test and get government approval for their drugs. These manufacturers are familiar to many Americans: Pfizer, Johnson & Johnson, Merck, Eli Lilly and Bristol Myers Squibb. In all, there are about a dozen major drug manufacturers.
Next drug manufacturers have to get their drugs on a health insurer’s approved drug list. This approved list is called a formulary. The list contains drugs that offer best health outcomes and the best returns for-profit health insurers, which own the biggest PBMs.
Drug manufacturers offer rebates and discounts to persuade health insurers to list their products on the insurers’ formularies. It’s unclear how much input actual doctors have in the creation of the formulary.
UnitedHealth, the country’s largest and most profitable health insurer, is also the largest employer of doctors in the country. The public knows UnitedHealth’s PBM by the name of OptumRx. This consolidation of the health chain increases the ability of the company to be gatekeepers of prescription drugs, the drug costs and availability for patients.
UnitedHealth has vaulted up the Fortune 100 charts in the last 20 years thanks to this consolidation and now ranks fourth behind WalMart, Amazon and Apple as the country’s most valuable companies. It is valued at $480 billion.
The health insurers and their PBMs also decide if they will allow generics onto their approved lists. To get on these approved lists, PBMs require rebates and discounts from the manufacturers.
Wholesalers purchase the drugs from manufacturers at an already set list price that they have negotiated with the manufacturers.They then distribute the drugs to pharmacies, hospitals and clinics. There are mainly three wholesalers in the U.S.: AmerisourceBergen, Cardinal Health, and McKesson Corporation.
Doctors are largely unaware of the backroom deals health insurers and their PBMs have made with drug manufacturers. Late last year Dr. Bruce A. Scott, president of the American Medical Association (AMA) sounded the alarm that behavior by health insurers and their PBMs are harming patients.
“The call for increased regulatory oversight of PBM business practices is overwhelmingly welcomed by physicians as a check against possible anticompetitive harm resulting from low competition and high vertical integration in the PBM industry,” Scott said.
Pharmacists across the country filled more than 5 billion prescriptions last year. In order to do that they are required by PBMs and health insurers to sign contracts to have access to patients. These contracts give pharmacists little control over the price paid for prescription drugs at their counters. Prices for drugs are set by your health insurer and its PBM. Customers can also pay different amounts for the same drug at the same pharmacy. Why?
Because…
[READ THE COMPLETE ARTICLE HERE]
